Constipation in chronic kidney disease
Constipation is a common health issue affecting all age groups of people with a higher rate of occurrence in older age group population. Constipation can reduce the quality of life and also social activities. Constipation is common problem in patients with chronic kidney disease (CKD) especially in those with advanced stage and those who are undergoing dialysis. Recent studies showed that constipation is associated with worsening of kidney function in patients with kidney disease, heart related events and mortality but confirmatory evidence is not yet available for the same.
How to diagnose constipation?
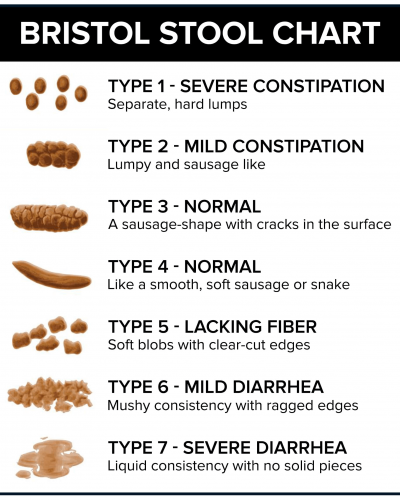
Constipation is change is bowel habits. Patients with constipation have less frequent stools (feces) usually less than 3 spontaneous stools per week. Stools can be difficult to pass and they can be lumpy or hard. There can be sensation of blockage at anus and incomplete evacuation. Simple and objective way to diagnose constipation is via Bristol Stool Form Scale as shown in the figure below. Type 1 stool is severe constipation and type 2 stool is mild constipation.
What are the reasons for constipation in CKD?
- Gut dysbiosis: It means change is the type of bacteria and function of bacteria in the intestines. In the intestines of patients with chronic constipation, good bacteria (e.g., Lactobacillus and Bifidobacterium genera) are decreased and problematic bacteria are increased. Good bacteria ferment the dietary plant derived carbohydrate to products which stimulate contraction of large intestine. As the good bacteria decreases constipation increases.
- Uremic toxins: Toxins accumulated in the body because of kidney dysfunction (also called as uremic toxins) cause motility problems in the large intestine leading to slow movement of stools. Large intestine receives approximately 1500ml of liquid from small intestine daily. Out of this, water and electrolytes are absorbed in large intestine and 200 – 400ml of water is excreted along with stools (feces). If there is slow movement in the large intestine, it will lead to more absorption of water and hard stools are formed which leads to constipation. As the stools stay for longer duration, amino acids in the stool are converted to uremic toxins which further affects the movement of stools leading to worsening of constipation.
- Life style: less physical activity in dialysis patients, improper use of laxatives and suppressing the urge to pass stools during dialysis sessions can promote constipation
- Medications: Blood pressure controlling medications (calcium channel blockers), potassium decreasing medications (resins), phosphorus controlling medications (e.g., sevelamer) and antidepressants can cause constipation
- Dietary restrictions: In advanced CKD, fiber rich vegetables and fruits are restricted for the fear of rise in potassium levels in blood. Water intake is also restricted particularly in patients on dialysis. Less fiber and fluid in the diet can cause constipation
Ways to deal with constipation?
Constipation in CKD patients is difficult to treat. The approach for treatment is multipronged targeting different aspects of etiology.
Life style and dietary changes
- Regular exercises like walking can be effective in improving constipation. Walking can promote bowel movements and relieve constipation.
- Movements in bowel are more after having meals. Making a routine to pass stools after meals can help people with constipation.
- Defecation posture change may help in relief in some patients. The classic Indian style toilet requires the person to squat while passing stools. Because of the position of squatting, pressure increases inside rectum and decreases at anus leading to easy passage of stools. It will lead to more faster and complete emptying of stools. Gradually Indian style toilets are becoming rare with western style sitting type of toilets becoming more common. We can get similar effect of squatting by using a foot stool in front of western type of toilet so that legs get flexed.
- Addition of vegetables and fruits with high fiber should be done after discussion with nephrologist and dietician and tailored based on the patient lab reports and requirements.
Probiotics and prebiotics
Probiotics are microorganisms which do benefit to the host on whom they reside. Prebiotics are components of food which are indigestible like fiber and complex starches which feed the probiotics. Studies done in patients with constipation and kidney disease have shown that supplementing prebiotics and probiotics have improved the constipation. Probiotics supplementation can be taken in the form of capsules after discussing with nephrologist. Probiotics are also available in other forms (e.g., yogurt). Before taking other forms of probiotics discussion with nephrologist and dietician is important because the source and dose to be taken of probiotics is important. For example, yogurt is derived from milk and excess milk product consumption in kidney failure patients is not recommended as it may increase phosphorus levels.
Laxatives
Laxatives are medications prescribed by doctors for the constipation. They are of various forms like syrup, liquid, powder or tablet. Commonly used laxatives are lactulose syrup which is available over the counter. Other commonly available laxatives like polyethylene glycol and psyllium need large quantity of water to be ingested along with them. Water restriction is important in the management of CKD patients so these options may not be best suited for them. Patients with kidney disease should be cautious about over the counter laxatives containing magnesium. Magnesium containing laxatives can lead to serious high levels of magnesium in the blood of these patients because kidneys in these patients cannot excrete the excess magnesium present in the laxative. If constipation is not relieved by life style modifications and changes in diet it is always necessary to contact the nephrologist for further medications before taking any over the counter preparations which are available.
Dr Kishore Kumar Ariga
Nephrologist and renal transplant physician
